Medicaid Insurance Coverage for Drug and Alcohol Rehab
One of the most common government-funded healthcare programs that support addiction treatment is Medicaid. It’s the main way individuals with little to no financial resources obtain the assistance they need for alcohol or substance abuse. Keep reading to learn more about rehabs that take Medicaid and how Medicaid can assist you or a loved one in paying for treatment.
Does your health insurance cover drug and alcohol treatment? Check your insurance.
Does Medicaid Insurance Cover Drug or Alcohol Rehab?
Yes, Medicaid insurance does cover drug and alcohol rehab for its members who require substance abuse and addiction treatment. Medicaid covers many other rehabilitation services, including detoxification, inpatient and outpatient rehab programs, and medication-assisted treatment. Besides covering rehabilitation treatment, you may wonder if Medicaid covers counseling and behavioral therapy. Depending on the specific plan, coverage may include cognitive-behavioral therapy (CBT), counseling, and aftercare support services for relapse prevention
Does Your Insurance Cover Rehab?
Find out your health insurance coverage levels for rehab treatment.
CALL (866)-461-3339
We accept most insurance plans and can check your coverage levels on your behalf.
Does Virtue Recovery Center accept Medicaid health insurance?
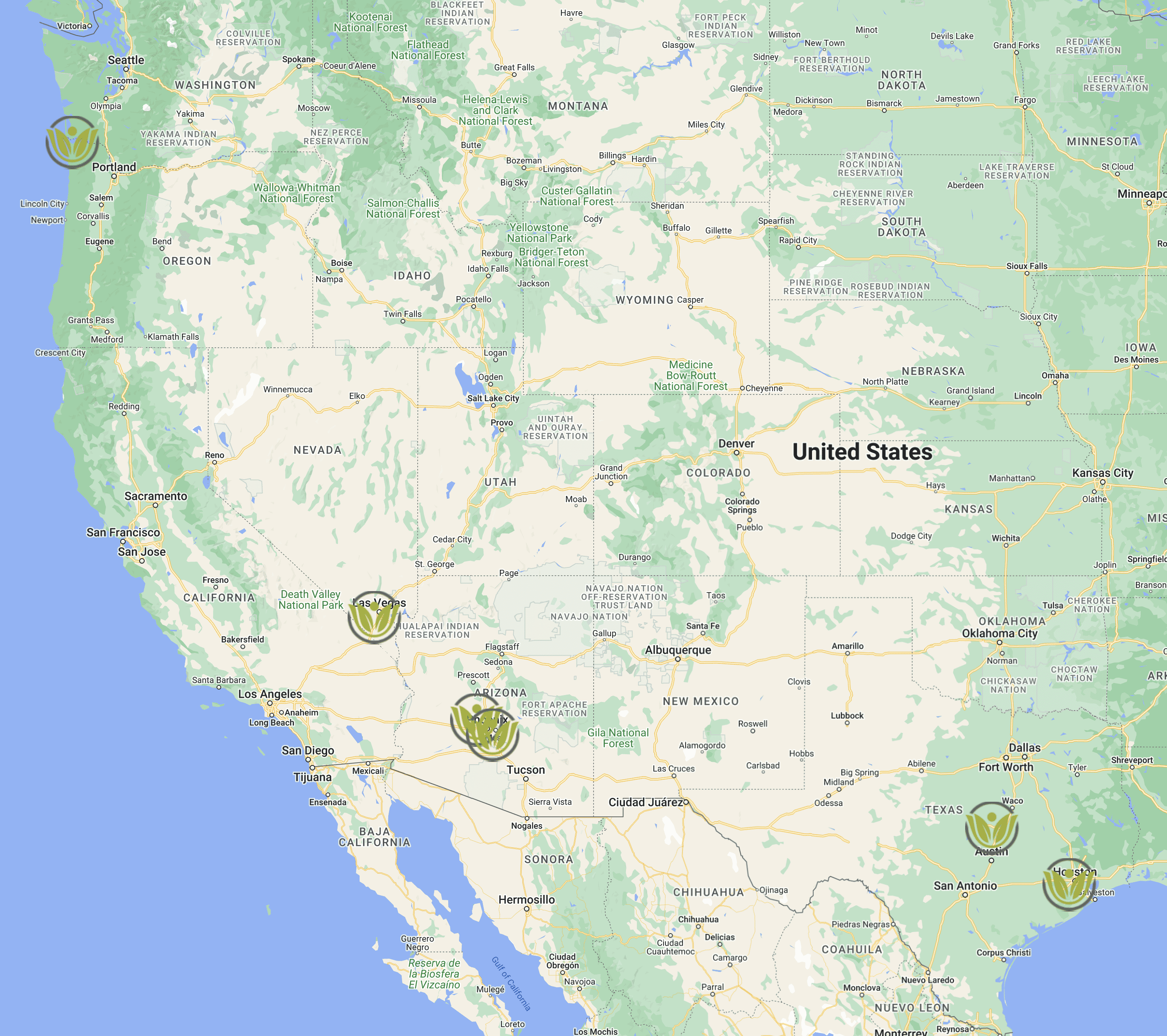
Yes, Virtue Recovery Center is in-network with Medicaid, a significant health insurance provider. This connection allows us to offer critical recovery services to individuals grappling with drug and alcohol addiction. If you hold Medicaid insurance and reside in Texas, Arizona, or Nevada, our centers in these locations may accept your insurance for treatment. Our priority is making our comprehensive recovery programs accessible to those who need them, and being in-network with Medicaid is a part of this commitment.
Our services encompass everything from detoxification programs, inpatient and outpatient rehab, and medication-assisted treatment. Each service is designed to provide you with the supportive, empathetic, and professional care you need on your road to sobriety. We are here to guide you every step of the way and ensure you have all the resources necessary for success. Your journey to recovery is our priority, and we are committed to helping you navigate it confidently.
-
Coverage
-
Does Medicaid Cover Mental Health Rehab?
In the US, Medicaid is the largest payer for mental health care.1 Under the Medicaid program, mental health services are considered a part of essential health benefits and are therefore covered. However, the extent of coverage and limitations can vary by state, so it’s best to call 866-461-3339 to determine the specifics of your Medicaid reimbursement.
Medicaid services for mental health rehab may include inpatient and outpatient care, psychotherapy such as cognitive-behavioral therapy, dual diagnosis, aftercare, medication management, support groups, and other services.
How Much Does Rehab Cost With Medicaid Health Insurance?
The average cost of inpatient rehab with Medicaid can vary depending on several factors, including the state where you live, your specific Medicaid plan, and the type of treatment you need. In general, Medicaid is designed to make rehab services more affordable and accessible to those who need them, including inpatient care.
According to a report from the Substance Abuse and Mental Health Services Administration (SAMHSA), the average cost of inpatient treatment for substance use disorders was $16,104 per stay in 2018.2 However, the actual cost of inpatient rehab with Medicaid can vary widely. In some cases, Medicaid may cover the total cost of rehab services, while in other cases, you may be responsible for copayments or a portion of the treatment cost.
How To Check My Medicaid Insurance Coverage Levels for Rehab Treatment
The best way to verify insurance details is by filling out our no-obligation online form or calling us at 866-461-3339. We’ll contact Medicaid directly and call you as soon as possible to review your policy details and discuss the next steps. Virtue Recovery Centers guarantees to keep any information exchanged entirely confidential.
-
Plan Types
-
Medicaid Insurance Plan Types
Medicaid members will have several options when choosing a Managed Care Organization (MCO) health plan.
MCO contractors now include:
• Anthem Blue Cross & Blue Shield
• Health Plan of Nevada
• Molina Healthcare of Nevada (New)
• SilverSummit Healthplan
Approximately 75 percent of Medicaid population receive medical benefits through an MCO. With the addition of a fourth MCO for 2022, the new contracts require Medicaid to distribute members equally among all the MCOs.
Medicaid members should ensure their contact information is up to date by calling the Division of Welfare and Supportive Services at 702-486-1646 or 1-800-992-0900. -
Insurance Overview
-
Medicaid is a joint federal and state program in the United States that provides access to healthcare coverage for low-income families and individuals. Created in 1965 under the Social Security Act and administered by the Centers for Medicare and Medicaid Services (CMS) at the federal level, state Medicaid programs must comply with federal guidelines.
The specific services from Medicaid vary by state, but they generally include the following:
- Doctor visits
- Hospital stays
- Prescription drug coverage
- Long-term care
- Laboratory and diagnostic testing
- Medical equipment and supplies
- Home health services
- Behavioral health services
The eligibility criteria for Medicaid can also vary by state, but some general guidelines apply nationwide. You must meet certain income and asset requirements to be eligible for Medicaid.1 Specifically, you must have a household income at or below a certain percentage of the federal poverty level (FPL). The FPL is updated annually and varies depending on your household size and the state you live in.2
Additionally, you must not have too many assets, as Medicaid is intended to help those with limited financial resources. Asset limits also vary by state.
In addition to income and asset requirements, eligibility for Medicaid can be based on other factors, such as age, disability, pregnancy, and citizenship or immigration status. For example, some state Medicaid programs cover individuals with disabilities, regardless of income.
It’s important to keep in mind that eligibility criteria can vary by state and that some states have Medicaid expansion under the Affordable Care Act (ACA) to cover more individuals.3 Under the ACA, states can expand Medicaid eligibility to include adults with incomes up to 138% of the FPL, regardless of age, disability, or other factors. As of 2021, 38 states and the District of Columbia have expanded Medicaid eligibility. This number is expected to rise in mid-2023.4
-
Insurance Statistics
-
Rehab Treatment and Insurance Statistics
Enrollment Numbers
- Total Medicaid/CHIP Enrollment (December 2022): 92.3 million, an increase of 21.2 million from February 20203.
- Estimated Medicaid/CHIP Enrollment (March 2023): Approximately 95 million3.
Expenditure
- U.S. Health Care Spending (2022): $4.5 trillion, with Medicaid accounting for a significant portion4.
- Medicaid’s Share of U.S. Health Care Spending (2019): About 16%18.
- Medicaid Expenditures for New Adult Group (2014-2015): Summary level expenditure data available, including a breakout for individuals that are newly eligible14.
Coverage Types
- Mandatory Benefits: Inpatient and outpatient hospital services, physician services, laboratory and x-ray services, home health services, etc. 8.
- Optional Benefits: Prescription drugs, case management, physical therapy, occupational therapy, etc. 8.
Demographic Information
-
Next Steps
-
Check Your Aetna Insurance Coverage With Virtue Recovery Center
If you’re committed to recovery, submit a request to one of our professional admission coordinators today using the form below. Before discussing the next steps, a coordinator will address any inquiries regarding our programs, including interacting directly with Aetna on your behalf to check your insurance coverage levels for drug or alcohol addiction rehab.
Does Medicaid Cover Mental Health Rehab?
In the US, Medicaid is the largest payer for mental health care.1 Under the Medicaid program, mental health services are considered a part of essential health benefits and are therefore covered. However, the extent of coverage and limitations can vary by state, so it’s best to call 866-461-3339 to determine the specifics of your Medicaid reimbursement.
Medicaid services for mental health rehab may include inpatient and outpatient care, psychotherapy such as cognitive-behavioral therapy, dual diagnosis, aftercare, medication management, support groups, and other services.
How Much Does Rehab Cost With Medicaid Health Insurance?
The average cost of inpatient rehab with Medicaid can vary depending on several factors, including the state where you live, your specific Medicaid plan, and the type of treatment you need. In general, Medicaid is designed to make rehab services more affordable and accessible to those who need them, including inpatient care.
According to a report from the Substance Abuse and Mental Health Services Administration (SAMHSA), the average cost of inpatient treatment for substance use disorders was $16,104 per stay in 2018.2 However, the actual cost of inpatient rehab with Medicaid can vary widely. In some cases, Medicaid may cover the total cost of rehab services, while in other cases, you may be responsible for copayments or a portion of the treatment cost.
How To Check My Medicaid Insurance Coverage Levels for Rehab Treatment
The best way to verify insurance details is by filling out our no-obligation online form or calling us at 866-461-3339. We’ll contact Medicaid directly and call you as soon as possible to review your policy details and discuss the next steps. Virtue Recovery Centers guarantees to keep any information exchanged entirely confidential.
Medicaid Insurance Plan Types
Medicaid members will have several options when choosing a Managed Care Organization (MCO) health plan.
MCO contractors now include:
• Anthem Blue Cross & Blue Shield
• Health Plan of Nevada
• Molina Healthcare of Nevada (New)
• SilverSummit Healthplan
Approximately 75 percent of Medicaid population receive medical benefits through an MCO. With the addition of a fourth MCO for 2022, the new contracts require Medicaid to distribute members equally among all the MCOs.
Medicaid members should ensure their contact information is up to date by calling the Division of Welfare and Supportive Services at 702-486-1646 or 1-800-992-0900.
Medicaid is a joint federal and state program in the United States that provides access to healthcare coverage for low-income families and individuals. Created in 1965 under the Social Security Act and administered by the Centers for Medicare and Medicaid Services (CMS) at the federal level, state Medicaid programs must comply with federal guidelines.
The specific services from Medicaid vary by state, but they generally include the following:
- Doctor visits
- Hospital stays
- Prescription drug coverage
- Long-term care
- Laboratory and diagnostic testing
- Medical equipment and supplies
- Home health services
- Behavioral health services
The eligibility criteria for Medicaid can also vary by state, but some general guidelines apply nationwide. You must meet certain income and asset requirements to be eligible for Medicaid.1 Specifically, you must have a household income at or below a certain percentage of the federal poverty level (FPL). The FPL is updated annually and varies depending on your household size and the state you live in.2
Additionally, you must not have too many assets, as Medicaid is intended to help those with limited financial resources. Asset limits also vary by state.
In addition to income and asset requirements, eligibility for Medicaid can be based on other factors, such as age, disability, pregnancy, and citizenship or immigration status. For example, some state Medicaid programs cover individuals with disabilities, regardless of income.
It’s important to keep in mind that eligibility criteria can vary by state and that some states have Medicaid expansion under the Affordable Care Act (ACA) to cover more individuals.3 Under the ACA, states can expand Medicaid eligibility to include adults with incomes up to 138% of the FPL, regardless of age, disability, or other factors. As of 2021, 38 states and the District of Columbia have expanded Medicaid eligibility. This number is expected to rise in mid-2023.4
Rehab Treatment and Insurance Statistics
Enrollment Numbers
- Total Medicaid/CHIP Enrollment (December 2022): 92.3 million, an increase of 21.2 million from February 20203.
- Estimated Medicaid/CHIP Enrollment (March 2023): Approximately 95 million3.
Expenditure
- U.S. Health Care Spending (2022): $4.5 trillion, with Medicaid accounting for a significant portion4.
- Medicaid’s Share of U.S. Health Care Spending (2019): About 16%18.
- Medicaid Expenditures for New Adult Group (2014-2015): Summary level expenditure data available, including a breakout for individuals that are newly eligible14.
Coverage Types
- Mandatory Benefits: Inpatient and outpatient hospital services, physician services, laboratory and x-ray services, home health services, etc. 8.
- Optional Benefits: Prescription drugs, case management, physical therapy, occupational therapy, etc. 8.
Demographic Information
Check Your Aetna Insurance Coverage With Virtue Recovery Center
If you’re committed to recovery, submit a request to one of our professional admission coordinators today using the form below. Before discussing the next steps, a coordinator will address any inquiries regarding our programs, including interacting directly with Aetna on your behalf to check your insurance coverage levels for drug or alcohol addiction rehab.
STEP 1
Using your Health Insurance Card, fill out all of the fields on the confidential form.
STEP 2
A member of our staff will contact your insurer to verify if your policy will cover your treatment
STEP 3
We will contact you promptly with the results of the verification and discuss the next steps
Frequently Asked Questions (FAQ)
Rehab insurance coverage is a type of health insurance that offers benefits to those seeking medical help for a wide range of issues ranging from substance abuse to mental health concerns. Many types of medical care can be covered by rehab insurances. Programs like detoxification, behavioral therapy, medication-assisted treatment, inpatient and outpatient therapies, and others may be covered by your current health insurance plan.
The level of coverage for rehab is dependent on many factors and may vary depending on the exact details of your policy, the benefits provided, and the specific treatment requirements. Rehab insurance coverage is available through employer-sponsored plans, government-sponsored plans like Medicaid, commercial health insurance policies, and combinations.
The process of getting Medicaid to pay for rehab treatment can vary depending on your specific Medicaid plan and the state you live in. To get Medicaid addiction treatment coverage, you’ll need to follow certain steps and meet certain criteria. Below are some general steps you can take:
- Check your Medicaid coverage: First, you must ensure that your plan covers rehab treatment. Call 866-461-3339 – Virtue Recovery Center can handle this for you.
- Get a diagnosis: You will need a diagnosis of a substance use disorder or a mental health condition to be eligible for rehab treatment. A healthcare provider, such as a doctor or a therapist, can typically provide a diagnosis.
- Find a rehab provider: You will need to find rehabs that accept Medicaid. You can search for providers on your state Medicaid agency’s website or by dialing 866-461-3339.
- for more information about Virtue Recovery Center’s treatment facilities.
- Get a referral: You may need a referral from your primary care provider or a specialist to receive rehab treatment. This can depend on your specific Medicaid plan and the type of treatment you need.
- Get prior authorization: Your Medicaid plan may require prior authorization for rehab treatment. This means you must get approval from your Medicaid provider before receiving treatment. Again, Virtue Recovery Center can assist with this step.
Attend treatment: Once you have met all the requirements, attend your rehab treatment program as your healthcare provider recommends.
The number of times that Medicaid will pay for rehab treatment can vary depending on your specific Medicaid plan and your state. Generally, Medicaid will cover rehab treatment as often as medically necessary to treat your substance use disorder or mental health condition.
The duration of coverage and the number of treatment sessions covered will depend on the severity of your condition and the treatment plan recommended by your healthcare provider. In some cases, Medicaid may only cover a certain number of days or sessions of treatment per year, while in other cases, Medicaid may cover an unlimited number of sessions.
Under the Medicaid program, drug and alcohol rehab treatment is typically covered under behavioral health services.5 These services may have specific limitations, such as the number of days or sessions covered, but they usually include outpatient and inpatient care, detoxification, counseling, and medication-assisted treatment. Call 866-461-3339 to determine the details and limitations of your state’s Medicaid program.
Yes, Aetna generally covers outpatient rehab for substance abuse, but the level of coverage can vary depending on the specific Aetna insurance plan you have. Coverage details, such as the extent of services provided and any potential out-of-pocket costs, can differ based on the plan’s terms and conditions.
Outpatient rehab services typically include therapies like counseling sessions, group therapy, educational sessions on substance abuse, and support for maintaining sobriety. To understand the specifics of your coverage for outpatient rehab, it’s essential to review your Aetna policy details or contact Aetna directly. They can provide the most accurate and personalized information regarding your eligibility for outpatient rehab services, coverage extent, and any prerequisites or conditions you need to meet.
Virtue Recovery Center has been saving individuals from drug and alcohol abuse and restoring families for years with multiple accredited treatment locations in several states. You can contact our rehab centers at 866-461-3339 to determine if they accept Medicaid health insurance.
Yes, Medicaid does cover rehabilitation services after a hospital stay. However, the specific treatments and extent of coverage can vary by state and individual policies. It’s important to note that there are guidelines for this coverage and there may be some costs not covered by insurance. Medicaid also covers drug and alcohol rehab services in some cases. Medicare also plays a significant role in covering rehab costs, offering coverage for up to 100 days in a skilled nursing facility. Always consult with your healthcare provider or hospital discharge planner to understand the specifics of what your Medicaid plan will cover.
Virtue Recovery Center provides treatment for substance abuse, mental health issues, and eating disorders. They offer a range of treatment options such as medical detox, residential treatment, outpatient services, and aftercare.
Yes, Virtue Recovery Center has specialized programs for veterans, first responders, and individuals with dual diagnoses. They offer tailored care for these populations, addressing specific needs such as trauma and job-related stress.
To access treatment, individuals can contact Virtue Recovery Center directly for a free confidential assessment. The center can also assist with insurance verification and travel arrangements for treatment.
Virtue Recovery Center offers high-end amenities and utilizes evidence-based treatment methods. Amenities include chef-prepared meals and state-of-the-art facilities. Therapies include cognitive behavioral therapy, dialectical behavioral therapy, and holistic approaches like mindfulness and art therapy.
Yes, Virtue Recovery Center is accredited by The Joint Commission, ensuring they meet high standards of care. Each facility is also licensed by the state where it’s located.
Virtue Recovery Center accepts most insurance policies and will verify coverage for treatment. They work with clients to coordinate payment plans based on insurance coverage.
You can go to rehab treatment without insurance. If your insurance does not cover the treatment you need on your path to sobriety, there is no need to be concerned. There are several ways to finance rehabilitation without insurance.
Most treatment centers are happy to offer their clients payment plans and other financial options. In addition, you may be able to pay for it using one or more of the different approaches listed below:
- Sliding Scale Fees: A person’s income determines the service costs. The lower your income, the less you’ll pay out-of-pocket.
- Community-based groups, nonprofits, or government-funded programs: These programs are usually inexpensive or free and can include a variety of treatments, such as therapy and detoxification. Simply do an Internet search for your state, county, or city to identify low-cost substance use disorder treatment and services in your area.
- Employee Assistance Programs (EAPs): If employed, your company may have an EAP offering addiction treatment services. EAPs are usually designed to provide support and resources for employees struggling with personal or professional issues.
- Faith-based programs: Some faith-based organizations offer treatment services to individuals seeking help with their addiction. They may incorporate religious or spiritual ideology into their treatment approach.
- Peer support groups: Groups like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) can provide a supportive community for your recovery. These support groups are usually free to attend and are a valuable source of support during the rehab and recovery process.
- Umbrella Policy: a specific insurance policy that extends the liability protection your other insurance plans cannot. Although an umbrella policy usually doesn’t cover addiction treatment, it might offer an added layer of protection for any liability claims resulting from addiction treatment.
Although you might be able to obtain addiction treatment through the above options without insurance, it’s crucial to remember that service accessibility and the level of care may vary significantly. Therefore, it is essential to do your research, speak with medical experts, and look for accredited treatment providers to ensure you receive the finest care possible.
Additionally, addiction treatment costs shouldn’t stop you from seeking appropriate therapies or recovery programs. Virtue Recovery Center wants to ensure you or a loved one receives the best care available if you or they are considering getting treatment for a drug or alcohol addiction. We’ll work with you to create an affordable payment plan for unexpected expenses.
If you’re committed to recovery, send a request to one of our qualified admissions coordinators today. Before going over the next steps, a coordinator will respond to any questions about our programs, including pricing and payment option details.
FREE ASSESSMENT
Get immediate treatment help now. 100% safe & confidential.
CALL (866)-461-3339
Contact us to schedule a free confidential assessment with a licensed clinician.
Empowering Your Path to Lasting Recovery Top Reasons to Choose Virtue Recovery Center
At Virtue Recovery Center, we understand that selecting the right addiction treatment facility is a crucial step toward your recovery. That’s why we’re committed to offering exceptional care that stands out in the realm of addiction recovery.
Our Success Rate
Virtue Recovery Center prides itself on its evidence-based approach and outstanding success rates. We continuously monitor and evaluate our treatment outcomes to ensure we are providing the best possible care, with success rates that surpass industry averages.
Commitment to Your Recovery
Our dedication to your long-term wellness is unwavering. If you successfully complete our comprehensive 90-day treatment program and face challenges post-treatment, we offer a complimentary 30-day return to our center to help get you back on track.
Accessibility and Inclusivity
We believe that everyone deserves the chance to recover, which is why we accept a wide range of insurance plans and offer various financing options. Our centers are strategically located to ensure that top-notch care is within reach for those in need.
Ongoing Support and Community
Recovery is a lifelong journey, and at Virtue Recovery Center, we are with you every step of the way. Beyond initial treatment, we provide extensive post-recovery support, including sober living options and a vibrant network of alumni, to help you maintain your sobriety and build a fulfilling life in recovery.
Real Stories of Hope and Healing from Virtue Recovery Center







Virtue Recovery Centers in Las Vegas offering every level of care to help those in need, to include substance use and eating disorders. 3 beautiful facilities with knowledgeable, caring, compassionate and dedicated staff who truly care. Medical, clinical, operational and dietary teams work together for the most positive outcomes. The Alumni program is beyond anything I have ever seen, offering support and encouragement after discharge for as long as needed. The facilities are beautiful, welcoming, and well maintained. The rooms are spacious and comfortable. The housekeeping staff is exceptional, and the food is incredible! Come take a tour and see for yourself. I would not send my loved ones anywhere else.
Patricia O'Connell
Customer Review from Las Vegas
Virtue is one of the nicest, newest, and cleanest facilities I’ve ever been at. It’s not beaten up and chaotic like all other places I’ve been to! It has a good energy, and positive vibe feeling of peace and serenity. Staff is kind too! It has been a breath of fresh air! Perfect for starting your brand new life!
Dwayne Brown
Customer Review from Las Vegas
I can honestly say that this place helped me with my SUD and changed my way of thinking. The staff are all so open and friendly and someone is always there to lend an ear or a helping hand. I’ve been to a few rehabs and they have been nothing compared to Virtue in how they were run, the therapy and therapists, and the fact that the staff all love their jobs and truly do care for you. If you need help, or someone you love needs help, then don’t waste time or money trying anywhere else.
Michelle Nguyen
Customer Review from Houston
I cannot say enough positive things about this place. I came in as a first-timer to a residential facility and brought along with me a multitude of mental health struggles and addictions that had had a handle on my life for a long time.
• The staff is beyond amazing and genuinely invested in the wellbeing of the clients.
• My therapist was by far the best I have ever seen and so easy to talk to; I left with a better understanding of myself than I’ve had in my entire life.
• My case manager was insanely kind and went above and beyond for me.
Erica Jones
Customer Review from Killeen
I hit a rough patch heading into the holidays and relapsed, so I went back to Virtue for help. I had gone to the facility in Vegas a while back, but for insurance reasons I had to go to Killeen. Yes! Virtue is that good of a facility it’s worth traveling to, Killeen provided transportation to and from Austin airport. Really the only thing different between the two facilities was the location. Killeen is definitely a 5-star treatment center, very clean with beautiful room and comfortable beds. The staff was amazing from housekeeping to the director! Their program is great with a nice mix of classes and free time, with plenty of activities to do. The food is really good too, provided by in house executive chefs! Just another shoutout to the staff, very caring, genuine and loving what they do! I had forgotten a couple of things when I had packed, and a staff member went personally to the store and picked up what I needed. You cannot go wrong by picking Virtue for your treatment! oh… also ask about “Tyrone Bingo” it’s a wonderful night of entertainment!! Big hearted thank you to all the staff, you’re all a blessing!! followed with the “Serenity Prayer.”
Andrew Neubauer
Customer Review from Killeen
Virtue is a special place. As soon as you arrive you are accepted as if you are family. The staff is beyond amazing. They are the definition of ride or die. They will go to the ends of the earth to make sure you have everything you need to be successful on your road to recovery. If you want a better life call them now, check in, and wait it out, because patience is a Virtue!!!!!!!
Thomas Porchia
Customer Review from Sun City West
Steven Killian
Customer Review from Killeen
Rehabs That May Accept Medicaid Insurance
Virtue Recovery Center operates a network of facilities across the country, offering comprehensive addiction and mental health care for you or your loved one in a supportive and healing environment.







Virtue Recovery Sun City West
13951 W Meeker Blvd, Sun City West, AZ 85375
Check Your Medicaid Insurance Coverage for Rehab Treatment
Find out your health insurance coverage levels for substance abuse rehabilitation programs. We are in-network with most health insurance providers and may accept your insurance plan too.
Inpatient and Outpatient Rehab Centers That Take Medicaid Insurance
With multiple treatment facilities in different states, Virtue Recovery Center has rescued people from substance abuse and restored families for years. The Joint Commission accredits all of our inpatient/outpatient centers. In addition, we are a member of the National Association of Addiction Treatment Providers (NAATP) and are HIPAA compliant while maintaining transparency and adherence to applicable laws and regulations.
Below you’ll find links to all of our treatment facilities:
-
Arizona
-
Do Drug and Alcohol Rehab Centers in Arizona Take Medicaid Insurance Policies?
While the cost of addiction rehab can be high, you may be able to use your Medicaid insurance to pay for drug rehab in Arizona. Many are unaware of the addition of health insurance as a financing option for these services. Continue reading to learn more about using Medicaid health to assist with addiction recovery treatment in Arizona.
Do Medicaid Insurance Plans Cover Drug and Alcohol Rehab in Arizona?
Medicaid insurance plans typically cover drug and alcohol rehab in Arizona. It is important to remember that the exact coverage level will depend on many factors, including, but not limited to, the details of your policy and treatment needs. Medicaid offers a wide range of insurance plans, including coverage for behavioral health and addiction treatment. These policies may cover inpatient and outpatient care, detoxification, counseling, medication-assisted treatment, and more.
Do Medicaid Insurance Plans Cover Mental Health Rehab in Arizona?
Medicaid health insurance policies generally cover mental health recovery options in Arizona. Medicaid has a variety plans, including those that provide coverage for behavioral health and mental health services. These Medicaid policies may cover a variety of care, including both inpatient and outpatient rehab options, counseling, medication management, and other specialized behavioral health care options.
The amount of coverage will vary from plan to plan according to many factors such as the type and level of treatment required and the who is providing the care.
Arizona Inpatient and Outpatient Rehab Centers That Take Medicaid Insurance Plans
Virtue Recovery Center has been saving lives from substance abuse with rehab facilities in several states, including two nationally accredited luxury sites in Arizona. These evidence-based inpatient drug and alcohol rehabilitation facilities provide residential care for those with addiction, dual diagnosis, and underlying trauma.
Below are links to our Arizona-based Virtue Recovery Centers:
How Much Does Rehab Cost in Arizona for Medicaid Insurance holders?
Arizona rehab costs for those with Medicaid insurance plans can vary based on a variety of factors, including which Medicaid insurance policy is held by the patient and the details of the the rehab program such as the type and length of treatment. Medicaid insurance plans often pay all or part of the rehab costs.
Depending on the level of coverage, only certain recovery options maybe covered or pre-treatment steps maybe required to be completed. For example, some Medicaid plans may need pre-authorization before covering services, while others may require care to be performed within a specific provider network.
The total cost of rehab is highly dependent of the type of treatment. For example, inpatient therapy requires a more extended stay at a facility and is often more expensive than outpatient therapy, which lets you continue living at home while receiving treatment. Inpatient rehab cost with insurance usually ranges from $5,000 to $25,000 or more.3 These are only averages that depend upon many variables.
How To Check Medicaid Coverage Levels in Arizona?
Virtue Recovery Center is happy to verify your insurance coverage levels with Medicaid for options in Arizona. Simply fill out our no-obligation online form, and allow one of our highly qualified staff members to eliminate the difficulties and wait times associated with calling your insurance provider. We’ll contact you as soon as possible to review your benefits and discuss the next steps.
Virtue Recovery Center is in-network with most major insurance plans, and we have all the answers to the common question: “Do Medicaid insurance plans cover rehab in Arizona?” In addition, you can rest assured that any information you provide or discuss is entirely confidential.
-
Nevada
-
Do Drug and Alcohol Rehab Centers in Nevada Take Aetna Insurance Policies?
It’s common to wonder if Aetna insurance plans cover rehab in Nevada. The short answer is yes, but the extent of coverage depends on many factors, including your policy and the necessary level of care. Below, we’ve provided all the information you need about Aetna insurance and how it can help you on the path to recovery.
Do Aetna Insurance Plans Cover Drug and Alcohol Rehab in Nevada?
The Affordable Care Act (ACA) requires almost all health plans, including those offered by Aetna, to cover essential health benefits.4 Mental and behavioral health services are considered essential health benefits, meaning your plan must provide some coverage for these services. However, the extent of your coverage may vary depending on several factors. These include where you receive treatment, the intensity and duration of your treatment, and your specific insurance policy. Our team is standing by to help you navigate the complexities of health insurance coverage. To start, you can verify your benefits or call 866-576-0737. We will keep your information completely confidential and will help determine your Aetna insurance benefits for rehabilitation in Nevada.
Do Aetna Insurance Plans Cover Mental Health Rehab in Nevada?
Aetna covers various evidence-based mental health services, such as inpatient and outpatient therapy, counseling, and psychiatric care. Along with services for conditions like post-traumatic stress disorder (PTSD), your Aetna mental health coverage may also include other services listed partially below:5
- Behavioral Therapy
- Medication Therapy
- Access to a personal care advocate
- Behavioral Health Evaluations
- 24/7/365 Telehealth6
- Prescription Drug Plans
- Support Groups for family members and caregivers
- Wellness Programs
Remember that the covered mental health rehabilitation services may vary from policy to policy.
Inpatient and Outpatient Rehab Centers in Nevada that Take Aetna Insurance Policies
We aim to help you achieve sustainable recovery and sobriety through tailor-made treatment. We believe in personalized care for every patient and offer up-to-date, evidence-based treatments for drug and alcohol addiction. We understand that each client has unique needs and challenges to overcome, and we adapt our approach accordingly.
We are proud to have several nationally accredited rehabilitation centers, including one in Nevada that is in-network with Aetna. Our team has dedicated years to helping individuals like you or your loved one on their journey toward recovery and improving their mental health.
Call 866-576-0737 today to schedule your free assessment or speak with an admissions coordinator. Rest assured that any information you provide will be kept 100% confidential.
You can also visit our website or our Nevada-based treatment facility:
How Much Does Rehab Cost in Nevada with an Aetna Insurance Policy?
The cost of addiction recovery in Nevada is determined by various factors such as the type of rehab program, treatment duration, and your particular Aetna policy details. On average, residential rehab costs around $62,530 per person, while a 30-day outpatient program costs approximately $1,626.7Please keep in mind that the costs mentioned above are only estimates and can vary significantly. At Virtue Recovery Center, we firmly believe that the price of rehabilitation should not discourage anyone from seeking the vital assistance they need. That is why we are committed to working with you to create a payment plan that suits your financial resources.
Start your path to recovery and sobriety today by calling 866-576-0737. You can also verify insurance via our free, confidential online form.
How To Check Aetna Coverage Levels in Nevada?
If you’re committed to recovering from addiction and need to verify insurance information, please call 866-576-0737. Our team is highly attentive and dedicated to providing kind, non-judgmental support. Alternatively, you can complete our online insurance verification form, linked below. There are no obligations, and it’s completely free and confidential. We know the cost and complexity of rehabilitation process is daunting, but know that we are here to help you or your loved one get the help they need to start their recovery journey.
How To Get Aetna to Pay for Rehab in Nevada
Getting Aetna Insurance to pay for rehab treatment in Nevada is made simple by calling 866-576-0737 for a thorough explanation of which services are covered under your insurance plan, any exclusions or limitations, and the ins and outs of the rehab process. Determining your insurance details is a critical first step to receiving rehabilitation benefits.
You should then begin your search for addiction recovery facilities. Look for rehab centers in your immediate area that are part of the Aetna provider network and offer the services and level of care you or your loved one needs. Choosing an in-network facility with your insurance provider is also essential for maximizing your coverage for affordable healthcare. Before undergoing rehab treatment, checking if pre-authorization is required based on your plan is important. Aetna will need information such as your diagnosis, treatment plan, and expected duration of stay to determine if the treatment is medically necessary. At Virtue Recovery Center, we can help you with any pre-authorization processes required for addiction recovery services.
Remember to follow the recommended treatment plan once you have obtained pre-authorization and have been approved for services. This will ensure that your insurance covers your treatment and that you achieve the best possible outcomes. Review your insurance claims once you have undergone treatment to ensure that all services have been accurately reflected. This will help you avoid being charged for anything your insurance policy should cover. If you notice any errors in the claims, contact your insurance provider immediately to file an appeal.
How Many Times Will Aetna Pay for Rehab in Nevada?
The number of times that Aetna will cover rehabilitation in Nevada depends on various factors, such as the type of program, the specific conditions of the policy, and medical necessity. Aetna typically provides coverage if rehabilitation is considered medically necessary, meaning treatment is needed for a particular condition or disorder.
Aetna may need to conduct regular assessments to confirm whether ongoing treatment and coverage are necessary. Additionally, the duration of your rehabilitation program may be limited by Aetna insurance. However, the limitations will vary depending on your policy terms, the type of program you are enrolled in, and your unique medical requirements. Aetna may allow for multiple rehabilitation treatments.
-
Texas
-
Do Drug and Alcohol Rehab Centers in Texas Take Aetna Insurance Policies?
Using your Aetna insurance to pay for drug rehab in Texas, where substance use disorders (SUDs) are common, is beneficial in lowering the total cost of treatment. However, many individuals might be unaware of the addition of health insurance as a financing option for these services. Below is all the information you’ll need about Aetna rehab insurance coverage in Texas.
Do Aetna Insurance Plans Cover Drug and Alcohol Rehab in Texas?
Aetna insurance plans typically cover drug and alcohol rehab in Texas. However, the extent of coverage may vary depending on several factors, including your particular policy and treatment needs. Aetna offers various plans, including coverage for behavioral health and substance abuse treatment. In addition, these plans may cover inpatient and outpatient care, detoxification, counseling, medication-assisted treatment, and more.
Do Aetna Insurance Plans Cover Mental Health Rehab in Texas?
Aetna insurance plans generally cover mental health rehab in Texas. Aetna offers various plans, including those that provide coverage for behavioral health and mental health treatment. These plans may include inpatient care and outpatient rehab services, counseling, medication management, and other forms of specialized care.
The extent of coverage will vary from plan to plan according to many factors, including the specific type of treatment needed and the provider.
Texas Inpatient and Outpatient Rehab Centers That Take Aetna Insurance Plans
Virtue Recovery Center has been saving lives from substance abuse with multiple treatment locations in several states, including two nationally accredited luxury facilities in Texas. These evidence-based inpatient drug and alcohol rehabilitation facilities provide residential care for those with addiction, dual diagnosis, and underlying trauma.
Below are links to our Texas-based Virtue Recovery Centers:
How Much Does Rehab Cost in Texas for Aetna Insurance holders?
Texas rehab costs for those insured by Aetna can vary based on many factors, including the particular Aetna insurance plan and the type and duration of the rehab program. Generally, Aetna insurance policies often pay all or part of the rehab costs.
There may be limits or restrictions on the types of covered programs. For example, some Aetna plans may require prior authorization before covering services, while others may have a specific network of providers that must be used.
Inpatient therapy requires a more extended stay at a treatment facility and is often more expensive than outpatient therapy, which lets you continue living at home while receiving treatment. The typical monthly cost of inpatient rehabilitation with insurance is usually estimated to range from $5,000 to $25,000 or more.3 Again, however, these are only averages that depend upon many variables.
How To Check Aetna Coverage Levels in Texas?
Virtue Recovery Center is happy to verify your insurance coverage levels with Aetna. Simply fill out our no-obligation online form, and allow one of our highly qualified staff members to eliminate the difficulties and wait times associated with calling your insurance provider. We’ll contact you as soon as possible to review your benefits and discuss the next steps.
Virtue Recovery Center is in-network with most major insurance plans, and we have all the answers to the common question: “Do Aetna insurance plans cover rehab in Texas?” In addition, you can rest assured that any information you provide or discuss is entirely confidential.
How Many Times Will Aetna Pay for Rehab in Texas?
The number of times Aetna will pay for rehab in Texas can vary depending on the specific Aetna insurance plan, your treatment needs, and the medical necessity. Aetna often pays for rehab as long as it is deemed medically necessary, indicating that therapy is required to address a particular condition or illness.
Aetna may also demand reevaluations regularly to assess ongoing medical necessity and coverage. There can also be restrictions on how long a rehab program is covered.
Do Drug and Alcohol Rehab Centers in Arizona Take Medicaid Insurance Policies?
While the cost of addiction rehab can be high, you may be able to use your Medicaid insurance to pay for drug rehab in Arizona. Many are unaware of the addition of health insurance as a financing option for these services. Continue reading to learn more about using Medicaid health to assist with addiction recovery treatment in Arizona.
Do Medicaid Insurance Plans Cover Drug and Alcohol Rehab in Arizona?
Medicaid insurance plans typically cover drug and alcohol rehab in Arizona. It is important to remember that the exact coverage level will depend on many factors, including, but not limited to, the details of your policy and treatment needs. Medicaid offers a wide range of insurance plans, including coverage for behavioral health and addiction treatment. These policies may cover inpatient and outpatient care, detoxification, counseling, medication-assisted treatment, and more.
Do Medicaid Insurance Plans Cover Mental Health Rehab in Arizona?
Medicaid health insurance policies generally cover mental health recovery options in Arizona. Medicaid has a variety plans, including those that provide coverage for behavioral health and mental health services. These Medicaid policies may cover a variety of care, including both inpatient and outpatient rehab options, counseling, medication management, and other specialized behavioral health care options.
The amount of coverage will vary from plan to plan according to many factors such as the type and level of treatment required and the who is providing the care.
Arizona Inpatient and Outpatient Rehab Centers That Take Medicaid Insurance Plans
Virtue Recovery Center has been saving lives from substance abuse with rehab facilities in several states, including two nationally accredited luxury sites in Arizona. These evidence-based inpatient drug and alcohol rehabilitation facilities provide residential care for those with addiction, dual diagnosis, and underlying trauma.
Below are links to our Arizona-based Virtue Recovery Centers:
How Much Does Rehab Cost in Arizona for Medicaid Insurance holders?
Arizona rehab costs for those with Medicaid insurance plans can vary based on a variety of factors, including which Medicaid insurance policy is held by the patient and the details of the the rehab program such as the type and length of treatment. Medicaid insurance plans often pay all or part of the rehab costs.
Depending on the level of coverage, only certain recovery options maybe covered or pre-treatment steps maybe required to be completed. For example, some Medicaid plans may need pre-authorization before covering services, while others may require care to be performed within a specific provider network.
The total cost of rehab is highly dependent of the type of treatment. For example, inpatient therapy requires a more extended stay at a facility and is often more expensive than outpatient therapy, which lets you continue living at home while receiving treatment. Inpatient rehab cost with insurance usually ranges from $5,000 to $25,000 or more.3 These are only averages that depend upon many variables.
How To Check Medicaid Coverage Levels in Arizona?
Virtue Recovery Center is happy to verify your insurance coverage levels with Medicaid for options in Arizona. Simply fill out our no-obligation online form, and allow one of our highly qualified staff members to eliminate the difficulties and wait times associated with calling your insurance provider. We’ll contact you as soon as possible to review your benefits and discuss the next steps.
Virtue Recovery Center is in-network with most major insurance plans, and we have all the answers to the common question: “Do Medicaid insurance plans cover rehab in Arizona?” In addition, you can rest assured that any information you provide or discuss is entirely confidential.
Do Drug and Alcohol Rehab Centers in Nevada Take Aetna Insurance Policies?
It’s common to wonder if Aetna insurance plans cover rehab in Nevada. The short answer is yes, but the extent of coverage depends on many factors, including your policy and the necessary level of care. Below, we’ve provided all the information you need about Aetna insurance and how it can help you on the path to recovery.
Do Aetna Insurance Plans Cover Drug and Alcohol Rehab in Nevada?
The Affordable Care Act (ACA) requires almost all health plans, including those offered by Aetna, to cover essential health benefits.4 Mental and behavioral health services are considered essential health benefits, meaning your plan must provide some coverage for these services. However, the extent of your coverage may vary depending on several factors. These include where you receive treatment, the intensity and duration of your treatment, and your specific insurance policy. Our team is standing by to help you navigate the complexities of health insurance coverage. To start, you can verify your benefits or call 866-576-0737. We will keep your information completely confidential and will help determine your Aetna insurance benefits for rehabilitation in Nevada.
Do Aetna Insurance Plans Cover Mental Health Rehab in Nevada?
Aetna covers various evidence-based mental health services, such as inpatient and outpatient therapy, counseling, and psychiatric care. Along with services for conditions like post-traumatic stress disorder (PTSD), your Aetna mental health coverage may also include other services listed partially below:5
- Behavioral Therapy
- Medication Therapy
- Access to a personal care advocate
- Behavioral Health Evaluations
- 24/7/365 Telehealth6
- Prescription Drug Plans
- Support Groups for family members and caregivers
- Wellness Programs
Remember that the covered mental health rehabilitation services may vary from policy to policy.
Inpatient and Outpatient Rehab Centers in Nevada that Take Aetna Insurance Policies
We aim to help you achieve sustainable recovery and sobriety through tailor-made treatment. We believe in personalized care for every patient and offer up-to-date, evidence-based treatments for drug and alcohol addiction. We understand that each client has unique needs and challenges to overcome, and we adapt our approach accordingly.
We are proud to have several nationally accredited rehabilitation centers, including one in Nevada that is in-network with Aetna. Our team has dedicated years to helping individuals like you or your loved one on their journey toward recovery and improving their mental health.
Call 866-576-0737 today to schedule your free assessment or speak with an admissions coordinator. Rest assured that any information you provide will be kept 100% confidential.
You can also visit our website or our Nevada-based treatment facility:
How Much Does Rehab Cost in Nevada with an Aetna Insurance Policy?
The cost of addiction recovery in Nevada is determined by various factors such as the type of rehab program, treatment duration, and your particular Aetna policy details. On average, residential rehab costs around $62,530 per person, while a 30-day outpatient program costs approximately $1,626.7Please keep in mind that the costs mentioned above are only estimates and can vary significantly. At Virtue Recovery Center, we firmly believe that the price of rehabilitation should not discourage anyone from seeking the vital assistance they need. That is why we are committed to working with you to create a payment plan that suits your financial resources.
Start your path to recovery and sobriety today by calling 866-576-0737. You can also verify insurance via our free, confidential online form.
How To Check Aetna Coverage Levels in Nevada?
If you’re committed to recovering from addiction and need to verify insurance information, please call 866-576-0737. Our team is highly attentive and dedicated to providing kind, non-judgmental support. Alternatively, you can complete our online insurance verification form, linked below. There are no obligations, and it’s completely free and confidential. We know the cost and complexity of rehabilitation process is daunting, but know that we are here to help you or your loved one get the help they need to start their recovery journey.
How To Get Aetna to Pay for Rehab in Nevada
Getting Aetna Insurance to pay for rehab treatment in Nevada is made simple by calling 866-576-0737 for a thorough explanation of which services are covered under your insurance plan, any exclusions or limitations, and the ins and outs of the rehab process. Determining your insurance details is a critical first step to receiving rehabilitation benefits.
You should then begin your search for addiction recovery facilities. Look for rehab centers in your immediate area that are part of the Aetna provider network and offer the services and level of care you or your loved one needs. Choosing an in-network facility with your insurance provider is also essential for maximizing your coverage for affordable healthcare. Before undergoing rehab treatment, checking if pre-authorization is required based on your plan is important. Aetna will need information such as your diagnosis, treatment plan, and expected duration of stay to determine if the treatment is medically necessary. At Virtue Recovery Center, we can help you with any pre-authorization processes required for addiction recovery services.
Remember to follow the recommended treatment plan once you have obtained pre-authorization and have been approved for services. This will ensure that your insurance covers your treatment and that you achieve the best possible outcomes. Review your insurance claims once you have undergone treatment to ensure that all services have been accurately reflected. This will help you avoid being charged for anything your insurance policy should cover. If you notice any errors in the claims, contact your insurance provider immediately to file an appeal.
How Many Times Will Aetna Pay for Rehab in Nevada?
The number of times that Aetna will cover rehabilitation in Nevada depends on various factors, such as the type of program, the specific conditions of the policy, and medical necessity. Aetna typically provides coverage if rehabilitation is considered medically necessary, meaning treatment is needed for a particular condition or disorder.
Aetna may need to conduct regular assessments to confirm whether ongoing treatment and coverage are necessary. Additionally, the duration of your rehabilitation program may be limited by Aetna insurance. However, the limitations will vary depending on your policy terms, the type of program you are enrolled in, and your unique medical requirements. Aetna may allow for multiple rehabilitation treatments.
Do Drug and Alcohol Rehab Centers in Texas Take Aetna Insurance Policies?
Using your Aetna insurance to pay for drug rehab in Texas, where substance use disorders (SUDs) are common, is beneficial in lowering the total cost of treatment. However, many individuals might be unaware of the addition of health insurance as a financing option for these services. Below is all the information you’ll need about Aetna rehab insurance coverage in Texas.
Do Aetna Insurance Plans Cover Drug and Alcohol Rehab in Texas?
Aetna insurance plans typically cover drug and alcohol rehab in Texas. However, the extent of coverage may vary depending on several factors, including your particular policy and treatment needs. Aetna offers various plans, including coverage for behavioral health and substance abuse treatment. In addition, these plans may cover inpatient and outpatient care, detoxification, counseling, medication-assisted treatment, and more.
Do Aetna Insurance Plans Cover Mental Health Rehab in Texas?
Aetna insurance plans generally cover mental health rehab in Texas. Aetna offers various plans, including those that provide coverage for behavioral health and mental health treatment. These plans may include inpatient care and outpatient rehab services, counseling, medication management, and other forms of specialized care.
The extent of coverage will vary from plan to plan according to many factors, including the specific type of treatment needed and the provider.
Texas Inpatient and Outpatient Rehab Centers That Take Aetna Insurance Plans
Virtue Recovery Center has been saving lives from substance abuse with multiple treatment locations in several states, including two nationally accredited luxury facilities in Texas. These evidence-based inpatient drug and alcohol rehabilitation facilities provide residential care for those with addiction, dual diagnosis, and underlying trauma.
Below are links to our Texas-based Virtue Recovery Centers:
How Much Does Rehab Cost in Texas for Aetna Insurance holders?
Texas rehab costs for those insured by Aetna can vary based on many factors, including the particular Aetna insurance plan and the type and duration of the rehab program. Generally, Aetna insurance policies often pay all or part of the rehab costs.
There may be limits or restrictions on the types of covered programs. For example, some Aetna plans may require prior authorization before covering services, while others may have a specific network of providers that must be used.
Inpatient therapy requires a more extended stay at a treatment facility and is often more expensive than outpatient therapy, which lets you continue living at home while receiving treatment. The typical monthly cost of inpatient rehabilitation with insurance is usually estimated to range from $5,000 to $25,000 or more.3 Again, however, these are only averages that depend upon many variables.
How To Check Aetna Coverage Levels in Texas?
Virtue Recovery Center is happy to verify your insurance coverage levels with Aetna. Simply fill out our no-obligation online form, and allow one of our highly qualified staff members to eliminate the difficulties and wait times associated with calling your insurance provider. We’ll contact you as soon as possible to review your benefits and discuss the next steps.
Virtue Recovery Center is in-network with most major insurance plans, and we have all the answers to the common question: “Do Aetna insurance plans cover rehab in Texas?” In addition, you can rest assured that any information you provide or discuss is entirely confidential.
How Many Times Will Aetna Pay for Rehab in Texas?
The number of times Aetna will pay for rehab in Texas can vary depending on the specific Aetna insurance plan, your treatment needs, and the medical necessity. Aetna often pays for rehab as long as it is deemed medically necessary, indicating that therapy is required to address a particular condition or illness.
Aetna may also demand reevaluations regularly to assess ongoing medical necessity and coverage. There can also be restrictions on how long a rehab program is covered.
- How Much Does Rehab Cost
- How To Pay For Rehab
- Dual Diagnosis Insurance
- Free Inpatient Rehab
- Inpatient Rehab Insurance
- Outpatient Rehab Insurance
- Luxury Rehab Insurance
- Sober Living Insurance
- Mental Health Rehab Insurance
- Rehabs That Take Insurance
- Rehabs That Allow Cell Phones
- Rehabs That Allow Pets
- [1] Stilkind, Joseph. “Average Cost of Drug Rehab [2023]: By Type, State and More.” NCDAS, 1 Jan. 2023, drugabusestatistics.org/cost-of-rehab
- [2] SAMHSA, Center for Behavioral Health Statistics and Quality. “Key Substance Use and Mental Health Indicators in the United States: Results From the 2019 National Survey on Drug Use and Health.” Substance Abuse and Mental Health Services Administration (SAMHSA), 2019, www.samhsa.gov/data/sites/default/files/reports/rpt29393/2019NSDUHFFRPDFWHTML/2019NSDUHFFR090120.htm.
- [3] U.S. Department of Health & Human Services. “FACING ADDICTION IN AMERICA: The Surgeon General’s Report on Alcohol, Drugs, and Health.” SurgeonGeneral.gov, 2016, addiction.surgeongeneral.gov/sites/default/files/surgeon-generals-report.pdf.
- [4] U.S. Department of Health and Human Services. “Key Substance Use and Mental Health Indicators in the United States: Results From the 2019 National Survey on Drug Use and Health.” Substance Abuse and Mental Health Services Administration, Sept. 2020, www.samhsa.gov/data/sites/default/files/reports/rpt29393/2019NSDUHFFRPDFWHTML/2019NSDUHFFR1PDFW090120.pdf.
- [5] “Substance Use Disorders.” Medicaid.gov, 2014, www.medicaid.gov/medicaid/benefits/behavioral-health-services/substance-use-disorders/index.html.
- [6] U.S. Department of Health and Human Services. “Access to Medications for Opioid Use Disorder (MOUD) Among Medicare Fee-for-Service Beneficiaries:: Influence of CARES Act Implementation (2020).” Centers for Medicare and Medicaid Services, Jan. 2022, www.cms.gov/files/document/data-highlight-jan-2022-opiod.pdf.
- [7] HHS Publication. “Medicaid Coverage of Medication-Assisted Treatment for Alcohol and Opioid Use Disorders and of Medication for the Reversal of Opioid Overdose.” Substance Abuse and Mental Health Services Administration, 2018, store.samhsa.gov/sites/default/files/d7/priv/medicaidfinancingmatreport_0.pdf.
- [8] “Trends and Statistics | National Institute on Drug Abuse.” National Institute on Drug Abuse, 23 Feb. 2023, nida.nih.gov/research-topics/trends-statistics.
START YOUR RECOVERY TODAY!
Contact Virtue Recovery Center 24/7 for inpatient treatment near you