WHAT ARE EATING DISORDERS?
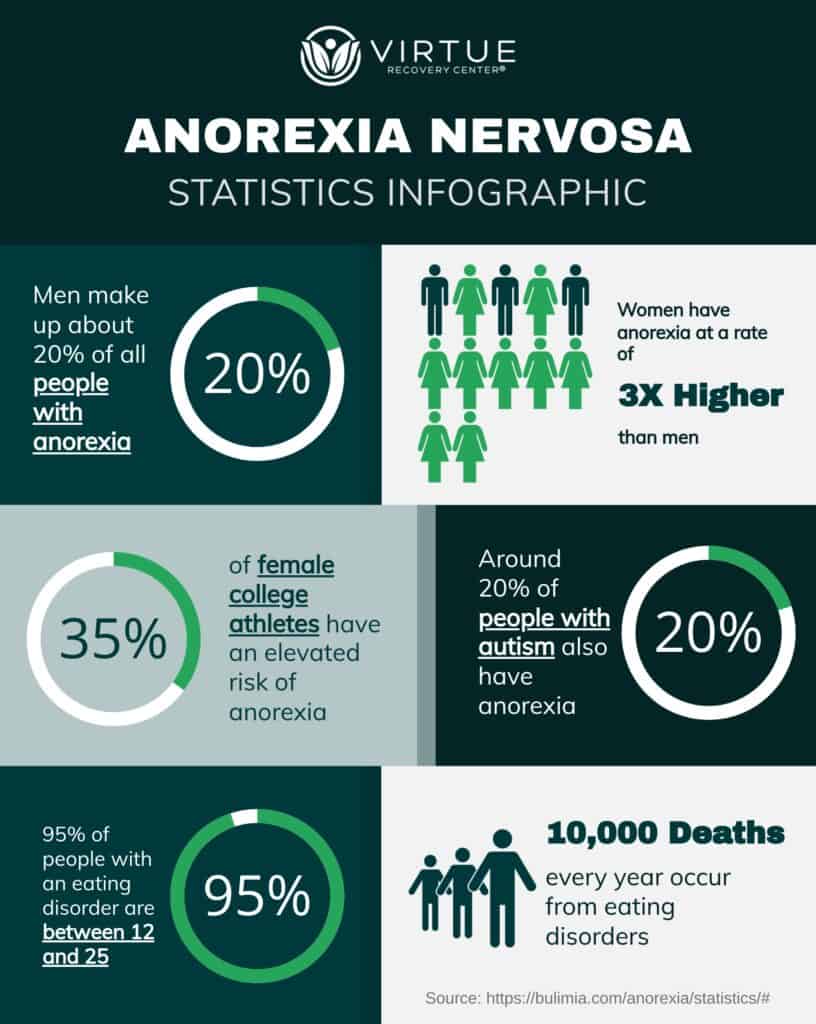
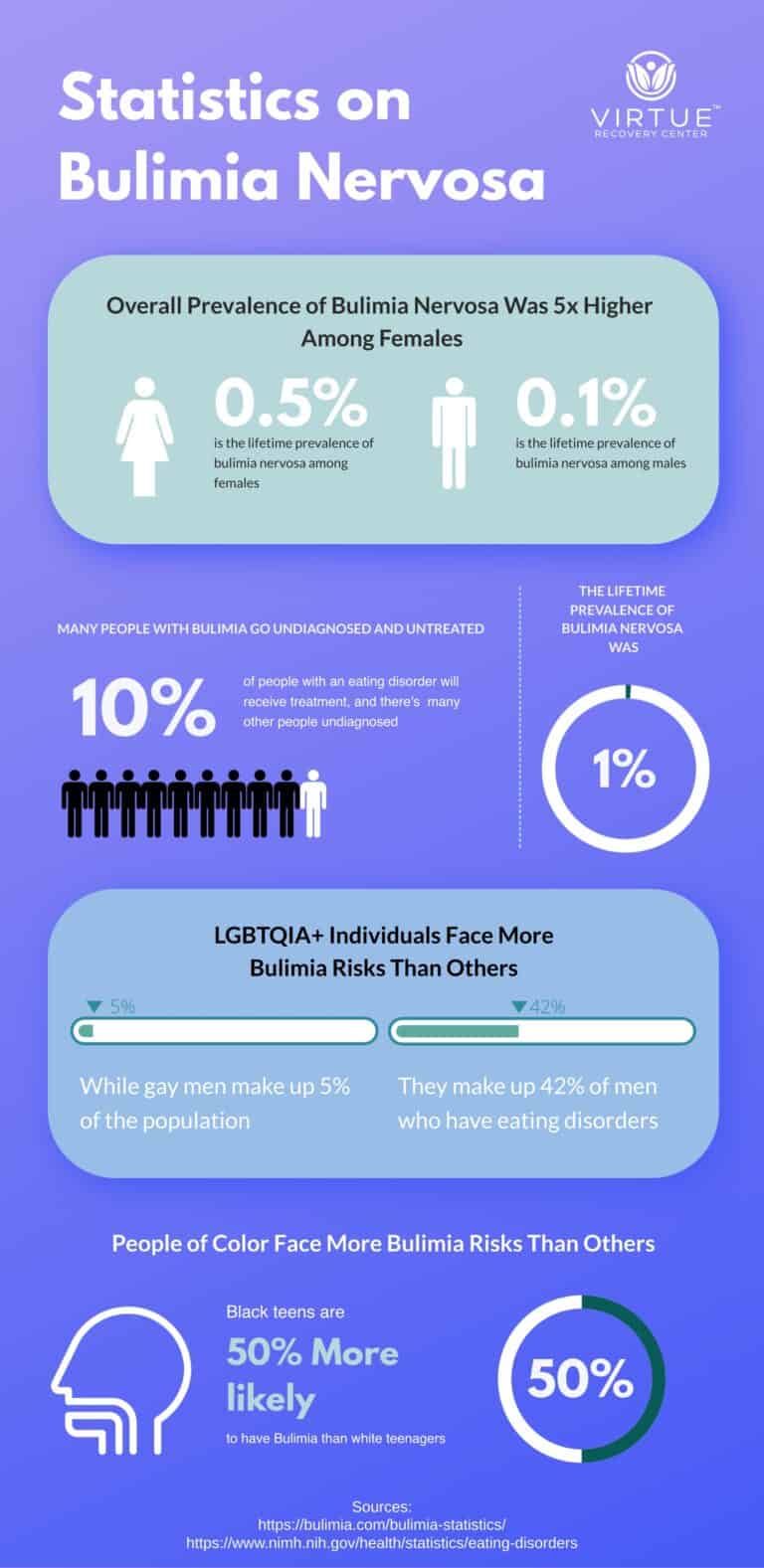
Eating disorders are complex mental health conditions characterized by unhealthy and often dangerous relationships with food, eating, and body image. These disorders can manifest in various forms, such as anorexia nervosa, bulimia nervosa, and binge-eating disorder, each with its own set of behaviors and symptoms. Individuals with eating disorders may obsess over food, weight, or body shape, leading to restrictive eating, purging, or binge-eating episodes. These behaviors can have severe physical and psychological consequences, affecting every aspect of a person’s life. Eating disorders often stem from a combination of genetic, environmental, psychological, and cultural factors, and they require comprehensive treatment that addresses both the underlying emotional issues and the physical health of the individual.